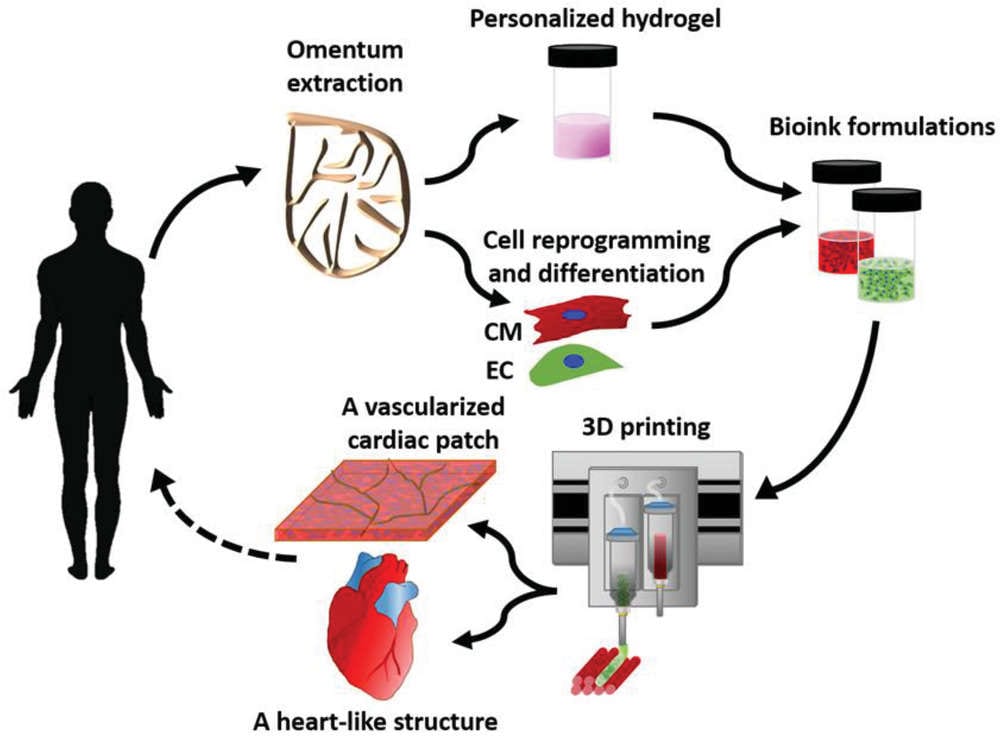
In an incredible breakthrough, researchers used a patient’s own cells and other biological materials to “completely match the immunological, cellular, biochemical, and anatomical properties of the patient.”
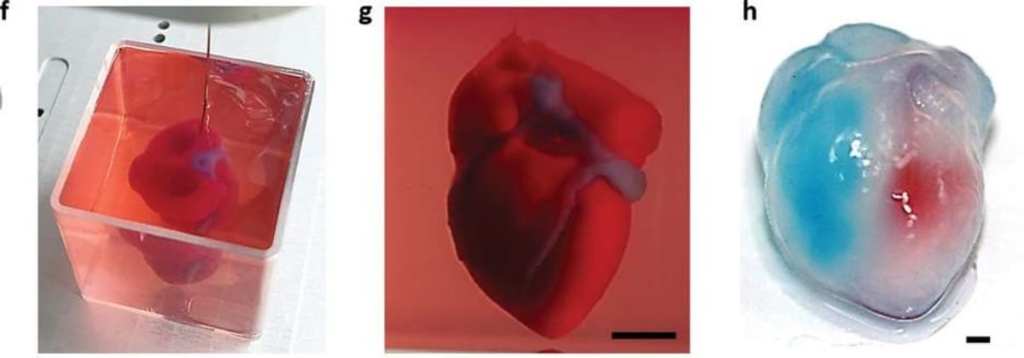
This is a big deal – until now, only simple tissues that lacked blood vessels have been 3D-printed.
The lead researchers issued a statement, and it’s easy to read their excitement between the lines.
“This heart is made from human cells and patient-specific biological materials. In our process these materials serve as the bioinks, substances made of sugars and proteins that can be used for 3D printing of complex tissue models. People have managed to 3D-print the structure of a heart in the past, but not with cells or with blood vessels. Our results demonstrate the potential of our approach for engineering personalized tissue and organ replacement in the future.”
The heart was made from fatty abdominal tissues which were reprogrammed to become pluripotent stem cells – “master cells” with the potential to produce any tissue or cell in the entire body.
Then they made the extracellular matrix – collagen and glycoproteins – into the printing “ink”. Once it mixed with the master cells, the ensuing slurry first grew into either cardiac or endothelial cells, then into patient-specific, immune-compatible cardiac patches with blood vessels, and then, amazingly, into an entire bioengineered heart.
The heart is not ready for human transplantation, though. Not yet.
Creating a fully functional human heart would take longer and require more cells – a billion or so – and the printed heart would have to be trained to pump like a real human heart. The ones they made have the ability to contract but not to work together in a coordinated pumping motion.
With heart disease being the leading cause of death in both men and women in the United States, the research is extremely exciting. Heart transplants work, but donors are in very short supply – not to mention that if hearts could be made from a patient’s own tissues, rejection would, in theory, be less of or not at all an issue.
“The biocompatibility of engineered materials is crucial to eliminating the risk of implant rejection, which jeopardizes the success of such treatments. Ideally, the biomaterial should possess the same biochemical, mechanical and topographical properties of the patient’s own tissues. Here, we can report a simple approach to 3D-printed thick, vascularized and perfusable cardiac tissues that completely match the immunological, cellular, biochemical and anatomical properties of the patient.”
The next step is to teach them to pump, then the team hopes to transplant them into animals for more testing.
What a time to be alive.