I have been obsessed (read: horrified but fascinated) with epidemics and the inevitable coming plague ever since I read The Hot Zone years ago. I couldn’t sleep for a week, and I still wash my hands obsessively – because I just know that something is going to pop up and wipe a good portion of us out at some point.
Image Credit: Amazon
In all of my reading and research, though, no one ever guessed that it could be a fungus.
Yet here we are.
The fungus – C. auris – was discovered in 2009 in the ear discharge (those two words are a good reason never to go into medicine, my friends) of a Japanese patient, though the earliest known strain dates back to South Korea in 1996.
Since then, it has spread through eastern and southern Asia, southern Africa, and South America. Cases have also emerged in the United Kingdom and other European countries, and are now on the rise in the U.S – 617 clinical cases so far this year.
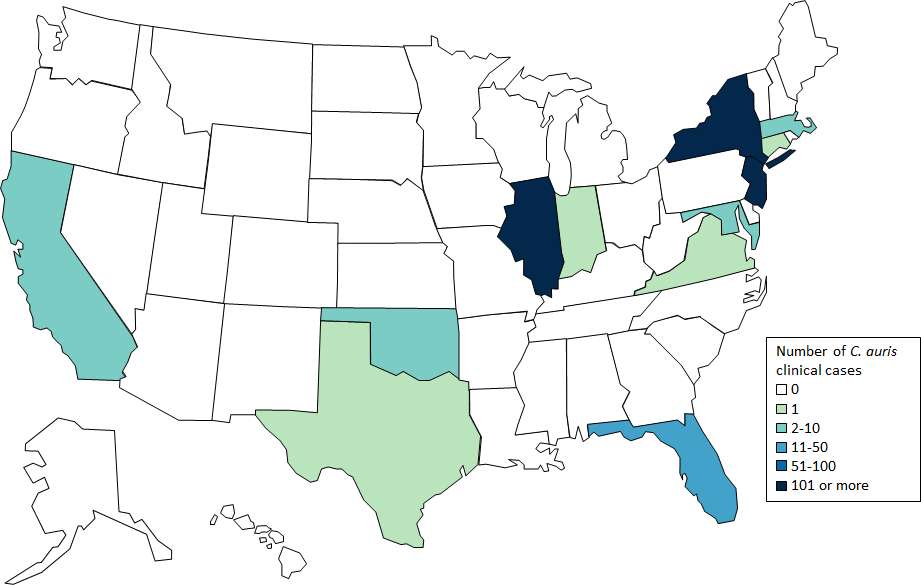
Image Credit: CDC
The CDC is calling the “relatively new and potentially deadly multidrug-resistant fungus” that is “spreading on a global scale” a serious threat.
Unlike normal yeast, which require warm, damp places to grow, Candida Auris can survive on cooler surfaces like skin and can remain there for a long time. This means it acts more like a bacteria than a fungus, but it’s not nearly as receptive to antibiotics as most bacterial infections.
The fungus can colonize its host for several months, or even indefinitely, without the potential patient showing any signs of infection, meaning that it can be transferred to objects and other humans without anyone being the wiser. Symptoms don’t typically appear until C. auris has entered the bloodstream and spread throughout the body, at which point invasive and difficult-to-treat infections arise.
It also doesn’t respond well to antifungals, or even the typical treatments used to cure vaginal yeast infections or oral thrush. Not only that, but it is extremely hard to kill on surfaces that have been in contact with an infected host – even hospitals where patients have stayed struggle to ensure no fungus has been left behind.
Okay, but should we really be that worried about a little fungus?
Maybe.
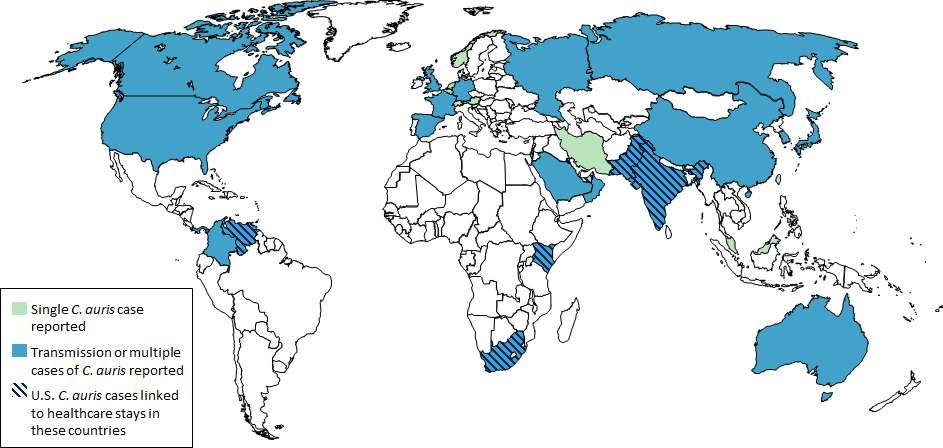
Image Credit: CDC
Right now, around 56,000 people in the US and EU die every year after contracting infections that are resistant to antibiotic treatment – about the same number of people who die from influenza, tuberculousis, and HIV/AIDS combined.
Those numbers are rising along with the number of bacteria – and now, fungus – that are growing a resistance to antibiotics. And while the CDC says the risk to otherwise healthy people is still low, those who have compromised immune systems definitely need to be cautious.
Welcome to the future, my friends. I hope you’ve read The Hunger Games.
And The Hot Zone.






